
Why women have Painful Sex (Dyspareunia)
Jun 28, 2021It can be a tough conversation to start. Often when patients raise the issue, “it” has been going on for a while. I’m talking about painful sex. It’s likely more common than you’d think, with estimates saying that nearly three out of four women experience painful intercourse at some point in their lives. Just because painful sex is common, that doesn’t mean you should accept it as "normal."
The Keys to Great Sex After Baby
Sex should be a pleasurable experience, and if it’s not, it is better to know why and what can be done to bring the pleasure back.
Dyspareunia happens in the pelvic area causing sharp or intense pain while having sex. It may cause women to experience intense or sharp pain and can happen while having intercourse and possibly before or after.
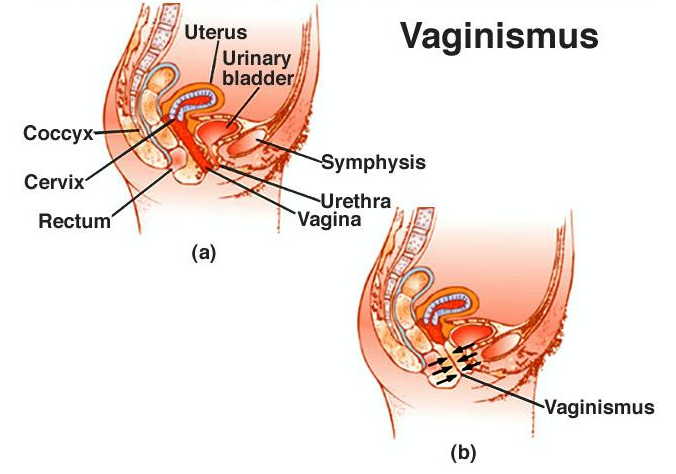
Vaginismus is a term referred to as involuntary tightening of the muscles at the entrance of the vagina. If a woman is nervous or feeling upset about having intimacy with her partner, this could make the body scream out loud, “NO ENTRY!” This condition could also occur if there is a physical problem caused by surgery or at birth.
Cases of vaginismus can range from mild to severe. In some cases, vaginismus tightness may begin to cause burning, pain, or stinging during intercourse. In other cases, penetration may be difficult or completely impossible.
What Causes Vaginismus?
The following are the most common causes of vaginismus in order of prevalence.
- Fear of pain, mostly because they heard from friends how painful it was for them
- Fear of the unknown
- Religious or cultural beliefs
- You perceive the vagina as fragile, thus worrying about scratching, hurting, breaking something inside it
- Past experience with discomfort, i.e., infection, a rough partner, a dry & uncomfortable vagina
While a woman may not know why she has vaginismus, she certainly knows that something is not right and may feel that she is inadequate or will never be able to have pleasurable sex.
The natural tendency is to suspect a medical problem, and, indeed, there are different potential medical causes for these problems, however, a better first line of defence would be a pelvic floor physical therapist. These professionals perform a thorough evaluation and assessment of the external and internal body parts and can determine if they need to refer on for medical input. More often than not, the condition is treatable by the pelvic floor therapist and the person can notice a change within a few sessions.
Could it be Stress?
Stress seems to be a contributing factor for everything these days but it is not to be taken lightly. Chronic underlying stress can contribute to inflammation in the body, and increase cortisol levels. High cortisol can decrease estrogen and lower estrogen can influence the tissues in the vagina such that they become dry and irritated. Stress can also contribute to tension in the pelvic floor muscles which can then play a role in sex being painful.
Some other causes of painful sex are:
- Vulvodynia—This is a pain disorder that affects the vulva. When pain is confined to the vestibule (the area around the opening of the vagina), it is known as vulvar vestibulitis syndrome (VVS).
- Hormonal changes—During perimenopause and menopause, decreasing levels of the female hormone estrogen may cause vaginal dryness.
- Vaginitis—Inflammation of the vagina, can be caused by a yeast or bacterial infection.
- Endometriosis. This is a condition in which the tissue similar to that which lines the uterus grows outside the uterus.
- Pelvic inflammatory disease (PID). With PID, the tissues deep inside become badly inflamed and the pressure of intercourse causes deep pain.
- Menopause. With menopause, the vaginal lining can lose its normal moisture and become dry.
How Can Painful Sex be Treated?
Many women with painful sex do not require medical treatment. If sex hurts, and especially if it hurts to the point that you are avoiding it or want to stop, it’s time to find a pelvic floor physical therapist and get help.
For cases of sexual pain in which there is no underlying medical or physical cause, working with a sexual health therapist may be beneficial.
Other Resources:
Recommended Programs:
The 28-Day Challenge and Buff Muff Membership
I recommend checking out my comprehensive pelvic health education and fitness programs on my Buff Muff App. The most complete Pelvic Floor & Kegel exercise App to strengthen the pelvic floor.
The Buff Muff 28-Day Challenge (housed in the App) gets you started, and the Annual membership keeps you progressing so you can laugh, run, jump, and lift without the pesky leaks and annoying discomfort of prolapse symptoms.




