Preparing For A Rectocele Repair – Prolapse Surgery
Dec 01, 2020My decision to have rectocele repair surgery was a BIG one and a lot of thought and research and care provider consults contributed to it. I feel a missing element of prolapse surgery is pre-hab and re-hab guidance. I hope to help change that with the aim of preventing surgery for some and improving the outcomes of those that go ahead. Here are some considerations for pre-op and post-op that may help you with your decision making and/or prep and recovery.
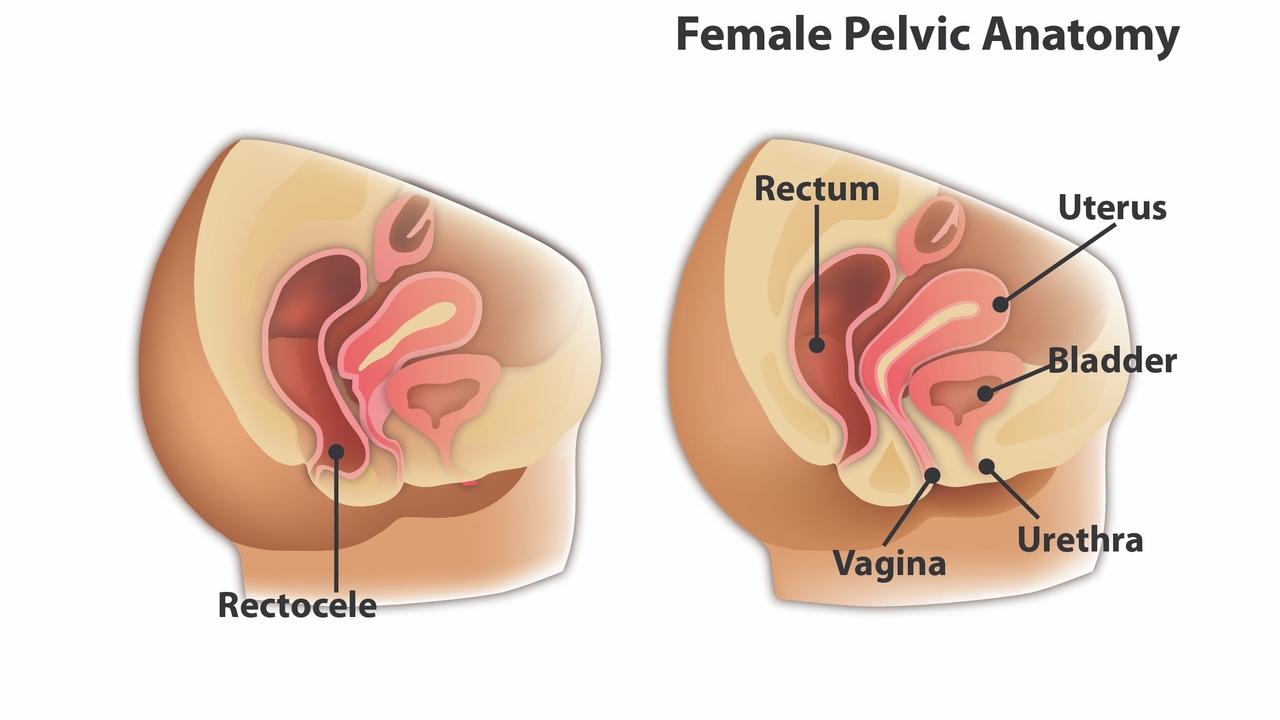
What is a rectocele?
A Rectocele is a type of prolapse indicated by the rectum bulging into the vagina. They can contribute to discomfort, difficulty voiding, feeling like ‘something is in there’, difficulty inserting a tampon or keeping it in. They can also be asymptomatic. Many people don’t even know they have a prolapse and the grade (1-4) of prolapse is not always indicative of the severity of or presence of symptoms.
What is a rectocele repair?
The most common rectocele repair is a repair of the posterior vaginal wall and is called a Posterior Colporrhaphy. An incision is made in the back wall of the vagina. The rectum is repositioned and the incision is sewn up while also reinforcing the walls of the vagina.
Does everyone need surgery?
Absolutely not. There are many conservative approaches to managing prolapse with diet and pelvic floor exercise being of utmost importance. Surgery is an option but one I recommend as a last resort. When a decision is made to have surgery, it is essential to consider pre-hab, working with a pelvic floor physical therapist and choosing the right surgeon.
How do you pick the best surgeon?
I recommend everyone with a vulva and a vagina see a pelvic floor physical therapist at least once a year. They can help you manage the conservative approaches to prolapse. Should you decide to have surgery, I suggest asking your pelvic floor physio who they recommend. They see the work of the surgeons and may have even worked with some. It is important to find a physio and a surgeon who you are comfortable with and who will help you navigate this big decision. I recommend seeking the opinion of more than one doctor to help determine the best fit for you.
What questions should I ask my surgeon?
I recommend using the B.R.A.I.N. acronym as a start.
- What are the Benefits?
- What are the Risks?
- What are the Alternatives?
- What is my Intuition?
- What if I do Nothing?
From there, I would like to know the name of the surgery, the length of the procedure, if it is native tissue or mesh, and how long it is estimated to last. I would also ask about how to prepare for it and how long recovery will take. Will you be off work? What if any lifting restrictions and for how long? Is there a recovery protocol to follow?
Should I do anything to prepare For rectocele repair Surgery?
Your doctor will have a preparation list such as the medication needed, an enema the night before but I believe outcomes could be improved with more intentional preparation. Working with a pelvic floor physiotherapist is one essential piece. Daily movement to help strengthen the pelvic floor (beyond just kegels) and also releasing tension in the muscles is important. Exercises like bridges, squats, deadlifts, one leg squats, walking and lunges are some key strengthening exercises. Supine butterfly, hamstring stretches, calf stretches, glute stretches and posterior pelvic floor release exercises are my picks for releasing tension.
I also recommend bringing a dildo with you to surgery. Yes, you read that correctly. Pain with sex is a possible challenge after a vaginal repair. One way I am choosing to help mitigate that risk is to bring a dildo with me to surgery that is roughly the same size as my husband's penis. The surgeon can then use it (sanitized) to ensure that there is not an over-correction.
I also recommend optimizing your diet ahead of time. Eat a low inflammatory diet and ensure constipation is not an issue prior to the surgery. Also, make sure you have a plan in place to help manage the first bowel movements. Having a rectocele repair to ‘help improve pooping’ is not wise. Get your bowel movements optimized first.
Drink a lot of water, eat 25-35 grams of fibre, move your body, get adequate rest and also ensure you prepare for your recovery.
What is the recovery like for a rectocele repair?
Typical recovery is 4-6 weeks with heavy lifting off-limits for at least 6 weeks. I will wait a lot longer than that and it will be a gradual return to more intense exercise. The challenge lies in the uninformed person who used to use symptoms to guide movement. Surgery can fix the symptom but doesn’t address what contributed to the problem developing in the first place. I recommend working with a pelvic floor physio ahead of time to address faulty or non-optimal movement patterns so they are not an ongoing issue after. Returning to exercise too soon, especially if the contributing factors to the prolapse have not been addressed is not recommended and can increase the chances of recurrence. Movement is recommended in the recovery to help with healing but take it slow and gradual.
Recovering from pelvic floor surgery is in many ways like postpartum recovery. The focus in the early days is rest and tissue supporting nutrition. I recommend perineal herbs to add to your sitz baths. I also recommend stool softeners for the first few days along with eating protein and foods that are easy to digest and supplements that help heal tissues (like Vitamin C). Some organic cotton pads will be needed and you can even soak a few in the perineal herbs and then freeze them (padsicles) to place on the perineum. A pair of underwear like the VieWear Underwear from Nyssa can help hold the frozen pads in place or have a pocket built in to hold a gel pack.
Gentle movement around the house later the first week and into the second coupled with some gentle movements like pelvic tilts and bridges may feel good. Listen and feel for any signs that it is too much. Bed rest is not recommended but overexertion isn’t either.
Pre-book a post-op assessment with your physiotherapist for around 8 weeks after your surgery. They can help gauge your readiness for more intense exercise and remember to see them annually going forward.
When can I return to fitness?
Much like it is advised to wait for 4-6 months postpartum to return to activities like running and jumping and heavy lifting, I view post-surgery the same. There needs to be a gradual, progressive return to these activities to ensure optimal movement patterns and load management. Ensuring your pelvic floor muscles have been retrained and are working well is essential before adding heavier loads and dynamic movements.
How can I ensure the best, longest-lasting outcome?
My parting words of wisdom;
- Work with a pelvic floor physical therapist
- Keep your diet and elimination optimized
- Be proactive as you approach menopause and consider local estrogen and/or DHEA supplementation
- Work to reduce inflammation in your body and support your immune system
- Choose exercise that builds your body instead of breaks it down
- There is more to pelvic floor wellness than kegels
- Sit less and move more
- Pay attention to your posture
- And see a pelvic floor physical therapist each year….wait, did I say that already? A few times? Yes, I did …because - It is THAT important.
Pelvic Surgery Success Program
Are you considering surgery as an option to feel like yourself again?
Pelvic Surgery Success is a one-of-a-kind program that will take you from feeling depressed, anxious, and consumed by fear of surgery to informed, confident and calm so you can put your nagging symptoms behind you and get back to living life with spontaneity and joy!
- Preparing For A Rectocele Repair – Prolapse Surgery
- Riding The Rollercoaster of Emotions – The Days Before Prolapse Surgery
- Post-Op Recovery The first few days - Prolapse Surgery - Rectocele Repair
- Post-Op Recovery Week 2 - Rectocele Repair - Prolapse Surgery
- Post-Op Recovery Week 3 - Rectocele Repair - Prolapse Surgery
- Post-Op Recovery Week 4 - Rectocele Repair - Prolapse Surgery
- Post-Op Recovery Week 5 - Prolapse Surgery - Rectocele Repair
- Post-Op Recovery Week 6 - Rectocele Repair - Prolapse Surgery
- Post-Op Recovery Week 7 - Rectocele Repair - Prolapse Surgery Check-In With My Pelvic Floor Physiotherapist



